Knowledge level of dental practitioners about obstructive sleep apnea
DOI:
https://doi.org/10.5281/zenodo.7562367Keywords:
Dentistry education, obstructive sleep apnea, oral appliancesAbstract
Objective: The importance of dentists in detecting and treating sleep disorders such as obstructive sleep apnea (OSA) and snoring is increasing daily. Therefore, dentists should have a good command of the clinical findings of OSA patients and should be included in the OSA treatment protocol when necessary. This study aims to measure dentists' level of knowledge about the diagnosis and treatment of OSA.
Materials and methods: A questionnaire was prepared using Google Forms WhatsApp to dentists in the 23-70 age range in Turkey, email and sent via Instagram and private social platforms like Facebook. The first part of the questionnaire contained basic questions providing demographic data, and the second part included questions about OSA. The data obtained were analyzed using the Statistical Package for Social Science version 23.0 (SPSS Inc., Chicago, IL, USA).
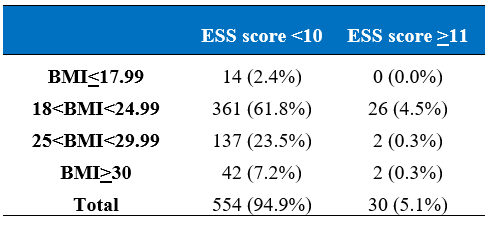
Results: A total of 584 dentists, 272 males, and 312 females, with a mean age of 29.45±5.88, participated in the survey. OSA knowledge scores of males were calculated as 11.87±4.65 and 12.20±4.23 for females. When the knowledge scores of 228 specialist dentists and 356 practitioners who participated in our study were compared, a statistically significant difference was found (p<0.05). It was determined that 30 (5.1%) of 584 participants had an ESS score of 11 or higher. It was concluded that 23.8% of the participants were overweight, and 7.5% were obese. No significant correlation was found between ESS scores and BMI values (p>0.05).
Conclusions: Although dentists do not have enough information about OSA diagnosis and treatment, they want to improve themselves on this issue. The dental education curriculum in Turkey is not sufficient for OSA. In light of our study, the dentistry curriculum can be updated and complementary training can be organized for graduate physicians.
References
Güneri P, İlhan B, Çal E, Epstein JB, Klasser GD. Obstructive sleep apnoea and the need for its introduction into dental curricula. Eur J Dent Educ.2017;21(2):121-9.
Freedman, N. Improvements in current treatments and emerging therapies for adult obstructive sleep apnea. F1000Prime Rep. 2014;6.
Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383(9918):736-47.
Greenstone M, Hack M. Obstructive sleep apnoea. Bmj, 2014;348:3745.
Prabhat KC, Goyal L, Bey A, Maheshwari S. Recent advances in the management of obstructive sleep apnea: The dental perspective. J Nat Sci Biol Med. 2012;3(2):113.
Al-Jewair TS, Nazir MA, Al-Masoud NN Alqahtani ND. Prevalence and risks of habitual snoring and obstructive sleep apnea symptoms in adult dental patients. Saudi Med J. 2016;37(2):183.
Swapna LA, Alotaibi NF, Falatah SA, Al Joaithen MS, Koppolu P. Knowledge of obstructive sleep apnea among dental fraternity in Riyadh. Open Access Maced J Med Sci. 2019;7(15):2508.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-5.
Lavanya R, Babu DBG, Chavva S, Boringi M, Waghray S, Yeladandi M. The role of oral physicians in predicting the risk of obstructive sleep apnea: A case-control study. Imaging Sci Dent. 2016;46(3):167-71.
Quan SF, Schmidt-Nowara W. The role of dentists in the diagnosis and treatment of obstructive sleep apnea: consensus and controversy. J Clin Sleep Med. 2017;1117-19.
Aarab G, Lobbezoo F, Heymans MW, Hamburger HL, Naeije M. Long-term follow-up of a randomized controlled trial of oral appliance therapy in obstructive sleep apnea. Respiration. 2011;82(2):162-8.
Jauhar S, Lyons MF, Banham SW, Orchardson R, Livingston E. The attitudes of general dental practitioners and medical specialists to the provision of intra–oral appliances for the management of snoring and sleep apnoea. Br Med J. 2008;205(12):653-7.
Bian H. Knowledge, opinions, and clinical experience of general practice dentists toward obstructive sleep apnea and oral appliances. Sleep Breat. 2004;8(2):85-90.
Taber KS. The use of Cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48(6):1273-96.
Ojeda IC, Jeffe DB, Guerrero T, Mantilla R, Santoro I, Gabino G, Cherrez A. Attitudes and knowledge about obstructive sleep apnea among Latin American primary care physicians. Sleep Med. 2013;14(10):973-7.
Smith HA, Smith ML. The role of dentists and primary care physicians in the care of patients with sleep-related breathing disorders. Front Public Health. 2017;5:137.
Baum BJ. Inadequate training in the biological sciences and medicine for dental students: an impending crisis for dentistry. J Am Dent Assoc. 2007;138(1):20.
Attanasio R, Bailey D. Dental Management of Sleep Disorders. 1st ed.;. Ames, IA: Wiley-Blackwell; 2010.
Vuorjoki‐Ranta TR, Lobbezoo F, Vehkalahti M, Tuomilehto H, Ahlberg J. Treatment of obstructive sleep apnoea patients in community dental care: knowledge and attitudes among general dental practitioners and specialist dentists. J Oral Rehabil.2016;43(12):937-42.
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479-504.
Faber J, Faber C and Faber AP. Obstructive sleep apnea in adults. Dental Press J. Orthod.2019;24(3):99-109.
Ng JH, Yow M. Oral appliances in the management of obstructive sleep apnea. Sleep Med Clin. 2019;14(1):109-18.
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. an American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2015;11(7):773-827.
Sharma S, Essick G, Schwartz D, Aronsky AJ. Sleep medicine care under one roof: a proposed model for integrating dentistry and medicine. J Clin Sleep Med. 2013;9(8);827-33.
Schotland HM, Jeffe DB. Development of the obstructive sleep apnea knowledge and attitudes (OSAKA) questionnaire. Sleep Med. 2003;4(5):443-50.
Marklund M, Braem MJ, Verbraecken J. Update on oral appliance therapy. Eur Respir Rev. 2019;28:153.
Ozoh OB, Iwuala SO, Desalu OO, Ojo OO, Okubadejo NU. An assessment of the knowledge and attitudes of graduating medical students in Lagos, Nigeria, regarding obstructive sleep apnea. Ann Am Thorac Soc. 2015;12(9):1358-63.
Al-Qattan H, Al-Omairah H, Al-Hashash K, Al-Mutairi F, Al-Mutairat M, Al-Ajmi M, Ziyab AH. Prevalence, risk factors, and comorbidities of obstructive sleep apnea risk among a working population in Kuwait: a cross-sectional study. Front in neurology. 2021;620799
Wetselaar P, Manfredini D, Ahlberg J, Johansson A, Aarab G, Papagianni CE, Lobbezoo F. Associations between tooth wear and dental sleep disorders: a narrative overview. J Oral Rehabil. 2019;46(8):765-75.
Heidsieck DS, Koolstra JH, de Ruiter MH, Hoekema A, de Lange J. Biomechanical effects of a mandibular advancement device on the temporomandibular joint. J Craniofac Surg. 2018;46(2):288-92.
Jokubauskas L, Pileičikienė G, Žekonis G, Baltrušaitytė A. Lithuanian dentists' knowledge, attitudes, and clinical practices regarding obstructive sleep apnea: A nationwide cross-sectional study. CRANIO®. 2019;37(4):238-45.
Kale SS, Kakodkar P, and Shetiya SH. Obstructive sleep apnea domains: Knowledge, attitude and practice results of dentists from a dental college in India. Sleep Sci. 2020;13(1):3.
Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, Guilleminault C. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev. 2017;36:57-70.
Prasad B, Steffen AD, Van Dongen HP, Pack FM, Strakovsky I, Staley B, Weaver TE. Determinants of sleepiness in obstructive sleep apnea. Sleep. 2018;41(2):zsx199.
Abrishami AA, Khajehdehi F, Chung A. Systematic review of screening questionnaires for obstructive sleep apnea. Can J Anesth. 2010;57(5):423-38.
Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7:467-72.
Walter TJ, Foldvary N, Mascha E, Dinner D, Golish J. Comparison of Epworth Sleepiness Scale scores by patients with obstructive sleep apnea and their bed partners. Sleep Med. 2002;3(1):29-32.
Gonsalves MA, Paiva T, Ramos E, Guilleminault C. Obstructive sleep apnea syndrome, sleepiness, and quality of life. Chest. 2004;125(6):2091-6.
Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep apnea in adults. JAMA. 2004;291(16):2013-6.
Bruno A, Pace E, Cibella F, Chanez P. Body mass index and comorbidities in adult severe asthmatics. BioMed Res Int. 2014;607192.
Cillo Jr JE, Thayer S, Dasheiff RM, Finn R. Relations between obstructive sleep apnea syndrome and specific cephalometric measurements, body mass index, and apnea-hypopnea index. Int J Oral Maxillofac Surg. 2012;70(4):e278-83.
Amra B, Rahmati B, Soltaninejad F, Feizi A. Screening questionnaires for obstructive sleep apnea: an updated systematic review. Oman Med J. 2018;33(3):184.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Journal of Clinical Trials and Experimental Investigations

This work is licensed under a Creative Commons Attribution 4.0 International License.
![]() The journal is licensed under a Attribution4.0 International (CC BY 4.0).
The journal is licensed under a Attribution4.0 International (CC BY 4.0).