Complications and difficulties due to bonesetter in the treatment of pediatric distal humerus fractures
DOI:
https://doi.org/10.5281/zenodo.7689647Keywords:
Neurovascular injury, supracondylar humerus fracture, traditional bonesetterAbstract
Objective: In this study, cases with delayed diagnosis and treatment due to traditional bonesetters were examined and in this article, we aimed to address the problems experienced by patients with supracondylar humerus fractures who were exposed to traditional bonesetters intervention and the physicians who treat these patients.
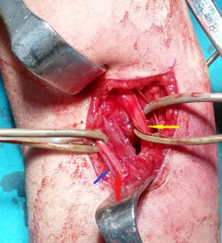
Materials and Methods: Thirty-six patients with supracondylar humerus fractures who were admitted to our hospital between January 2017 and December 2020 and were accepted as bonesetters sequelae were retrospectively reviewed. The time between injury and admission to the hospital, skin problems, neurovascular examinations, and soft tissue conditions of the patients were evaluated. The operation time, open or closed reduction, and fixation technique were examined.
Results: The mean time between fracture and admission to the hospital was 5.28 days (1-15 days). After the patients were admitted to the hospital, their surgeries were delayed due to edema or skin problems and delayed an average of 15.4 hours (5-48 hours). The mean operative time was 96.3 minutes (38-221 minutes), and 19 patients (52.8%) required open reduction. The mean hospital stay of the patients was 3 days (2-11 days). In the pre-operative evaluation, nerve lesion was detected in 6 patients (16.7%). It is remarkable that the number of patients who applied to our hospital after bonesetters applied in 2020, has increased significantly.
Conclusions: The application of bonesetters in children with fractures around the elbow causes a delay in the arrival of patients to the hospital and causes increased complications. The number of applications for bonesetters increased significantly in 2020 due to both the pandemic restrictions and the patients' avoidance of applying to the hospital during the COVID-19 pandemic. Edema and skin lesions as to dislocation sequelae affect the timing of Surgery.
References
Klimkiewicz JJ, Bradley JP, Sawyer JR. Pediatric elbow fractures and dislocations. In: DeLee D, editor. Orthopaedic sports medicine. Principles and practice. 2nd ed., Vol. 1. Philadelphia: Saunders; 2003.
Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop. 1999;19(3):344–50.
Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand. 1986;57(4):309-12.
Ramachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: the experience of a specialist referral center. J Bone Joint Surg Br. 2006;88(1):90-4.
Kara A. A review of childhood anxiety. J Clin Trials Exp Investig. 2022;1(3):64-70.
Omololu B, Ogunlade SO, Alonge TO. The complications seen from the treatment by traditional bonesetters. West Afr J Med. 2002;21(4):335-7.
Alemdar C, Azboy İ, Demirtaş A ve ark. Bölgemizdeki kırıkçı sekellerinin ortopedik açıdan değerlendirilmesi. İstanbul Med J. 2014;15:122-6.
Gözen A, Doğan A, Gökalp MA, Ünsal SŞ, Güner S. 2008-2012 yılları arasında sınıkçı müdahalesi sonrasında kliniğimize başvuran hastaların analizi. Tıp Araştırmaları Dergisi. 2015;13(1):15-9.
Özkul E, Gem M, Alemdar C, Arslan H, Azboy İ, Çelik V. Çocuklarda suprakondiller humerus kırığı sonrası damarsal yaralanmalar. Ulus Travma Acil Cerrahi Derg. 2016;22(1): 84-9.
Cambon-Binder A, Jehanno P, Tribout L, Valenti P, Simon AL, Ilharreborde B, et al. Pulseless supracondylar humeral fractures in children: vascular complications in a ten year series. Int Orthop. 2018;42(4):891-9.
Leiblein M, Lustenberger T, Schulz AK, Schmitz-Rixen T, Marzi I. Neurovascular complications after supracondylar humerus fractures in children. Trauma Case Rep. 2017;8:16–9.
Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop. 2010;30(3):253-63.
Garbuz DS, Leitch K, Wright JG. Treatment of supracondylar fractures with an absent radial pulse. J Paediatr Orthop. 1997;17(3):303-10.
Duffy S, Flannery O, Gelfer Y. Monsel F. Overview of the contemporary management of supracondylar humeral fractures in children. Eur J Orthop Surg Traumatol. 2021;31:871–81.
DeFrancesco CJ, Shah AS, Brusalis CM, Flynn K, Leddy K, Flynn JM. Rate of Open Reduction for Supracondylar Humerus Fractures Varies Across Pediatric Orthopaedic Surgeons: A Single-Institution Analysis. J Orthop Trauma. 2018;32(10):400-7.
Holt JB, Glass NA, Bedard NA, Weinstein SL, Shah AS. Emerging U.S. National Trends in the Treatment of Pediatric Supracondylar Humeral Fractures. J Bone Joint Surg Am. 2017;99(8):681-7.
Yildirim AO, Unal VS, Oken OF, Gulcek M, Ozsular M, Ucaner A. Timing of surgical treatment for type III supracondylar humerus fractures in pediatric patients. J Child Orthop. 2009;3(4):265-9.
Loizou CL, Simillis C, Hutchinson JR. A systematic review of early versus delayed treatment for type III supracondylar humeral fractures in children. Injury. 2009;40(3):245–8.
Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg (Br). 2006;88(4):528–30.
Abbott MD, Buchler L, Loder RT, Caltoum CB. Gartland type III supracondylar humerus fractures: outcome and complications as related to operative timing and pin configuration. J Child Orthop. 2014;8(6):473-7.
Sibinski M, Sharma H, Bennet GC. Early versus delayed treatment of extension type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg (Br). 2006;88(3):380–1
Striano BM, Brusalis CM, Flynn JM, Talwar D, Shah AS. Operative Time and Cost Vary by Surgeon: An Analysis of Supracondylar Humerus Fractures in Children. Orthopedics. 2019;42(3):e317-e321.
Shon HC, Kim JW, Shin HK, Eugene K, Park SJ, Park JK et al. Does the timing of surgery affect outcomes of gartland type III supracondylar fractures in children? Pediatr. Traumatol. Orthop. Reconstr. Surg. 2019;7:25–32.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Journal of Clinical Trials and Experimental Investigations

This work is licensed under a Creative Commons Attribution 4.0 International License.
![]() The journal is licensed under a Attribution4.0 International (CC BY 4.0).
The journal is licensed under a Attribution4.0 International (CC BY 4.0).